Management of CKD-associated Pruritus (formerly known as uremic pruritus) should be an essential part of treatment for all patients undergoing haemodialysis and suffering from this condition.1
Effective management of CKD-associated Pruritus could make a difference to patients.
Managing CKD-associated Pruritus can be a challenge, but is a challenge worth taking on. The treatment approach should be multifaceted and tailored to each patient’s dialysis goals.1,2

One of the first steps in the management of CKD-associated Pruritus is typically to ensure adequate dialysis through increasing dialysis dose (Kt/V), normalising calcium-phosphate balance and controlling parathyroid hormone (PTH) to accepted levels.1
Increase Kt/V
It is proposed that this strategy lowers the levels of pruritogens in the body. However, no target Kt/V is available to guide treatment.1,3,4
Normalise calcium-phosphate balance
Phosphorus control was ranked as the most important therapeutic option for severe pruritus overall by 60% of medical directors in DOPPS, likely as calcium and phosphate levels are often elevated in dialysis patients.2,5,6 Yet, once again, guidelines do not provide target levels for treatment.1,3,4
Control PTH to accepted levels
PTH causes renal tubular reabsorption of phosphorus and regulates blood phosphorus levels. Moreover, PTH in dialysis patients with itching is often reported as significantly higher than those in people without itching.2,6
However, despite the above rationale, these treatment options may not be sufficient given the multifactorial pathogenesis of CKD-associated Pruritus. A multivariate analysis of 6,256 patients from DOPPS found no association between CKD-associated Pruritus and Kt/V, phosphorus, calcium, calcium-phosphorus product, PTH, or hemodiafiltration.5
Patient characteristics according to the extent to which patients were bothered by itchy skin
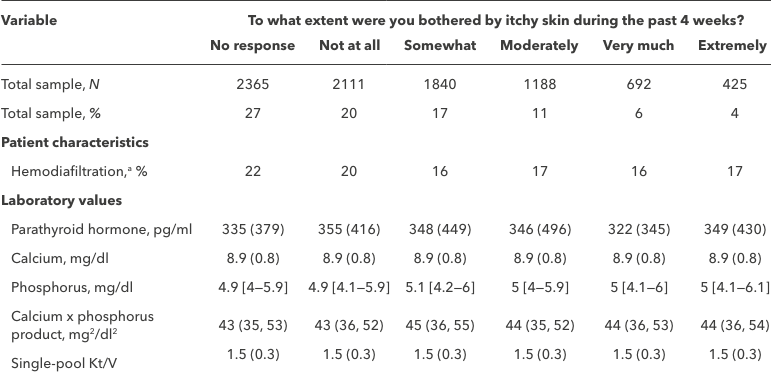
Adapted from: Rayner et al. 20175
Data are shown as mean (SD), median [interquartile range], or column percentage.
aHemodiafiltration excludes the United States and Canada due to lack of use (n=6024).
Xerosis occurs in up to 85% of dialysis patients, and although not thought to be the cause of CKD‑associated Pruritus, it likely contributes to its severity.2
Evidence supports treating patients with xerosis with emollients first, and to consider additional treatments, if pruritus persists.1,2
General principles from a position paper on the treatment of xerosis state that the drier the skin is (scaling/wrinkling/fissures), the more lipids are required. Whereas the more inflamed the skin is (erythema/pruritus), the higher the water content needs to be.7
Although mortality and life expectancy are important, in addition patients value the measures to improve the quality of their lives and in particular, the relief of symptoms associated with their treatment.4
CKD-associated Pruritus is associated with burdensome symptoms, which can diminish a patient’s quality of life. However, most symptoms and adverse effects currently lack approved treatments, and there is no existing tool that monitors symptoms over time.4
Agarwal et al. detail how understanding the pathophysiology of CKD-associated Pruritus resulted in the design, development and regulatory approval of a treatment for its relief.4
An algorithm has been proposed for the screening, diagnosis, assessment and treatment of CKD-associated Pruritus among patients undergoing haemodialysis. This algorithm considers the level of itch intensity and the impact of the itch on the patient’s quality of lifel.4
*Treatment selection dependent on the availability of difelikefalin.
To identify and assess CKD-associated Pruritus, patients should be asked if they itch every 3 months and be encouraged to rate their itch intensity using the Worst Itch Intensity – Numerical Rating Scale (WI-NRS).
Identifying CKD-aP
Watch this video for a description of how to use the WI-RNS to identify CKD-aP by surveying patients, assess itch intensity and understand the impact on patients’ quality of life through patient profiles.
CKD-associated Pruritus could have life-changing consequences for your haemodialysis patients, don’t
let them suffer in silence.
- Millington G, Collins A, Lovell C, et al. British Association of Dermatologists’ guidelines for the investigation and management of generalised pruritus in adults without an underlying dermatosis, 2018. Br J Dermatol. (2018);178(1):34–60.
- Verduzco H, Shirazian S. CKD-associated pruritus: new insights into diagnosis, pathogenesis, and management. Kidney Int Rep. (2020);5(9):1387–1402.
- Osakwe N, Hashmi MF. Uremic pruritus evaluation and treatment. StatPearls [Internet]. Last updated: February 2023. Available at: https://www.ncbi.nlm.nih.gov/books/NBK587340/. Accessed: June 2023.
- Agarwal R, Burton J, Gallieni M, et al. Alleviating symptoms in patients undergoing long-term hemodialysis: a focus on chronic kidney disease-associated pruritus. Clin Kidney J. (2023);16(1):30–40.
- Rayner H, Larkina M, Wang M, et al. International comparisons of prevalence, awareness, and treatment of pruritus in people on hemodialysis. Clin J Am Soc Nephrol. (2017);12:2000–2007.
- Hu T, Wang B, Liao X, et al. Clinical features and risk factors of pruritus in patients with chronic renal failure. Exp Ther Med. (2019);18(2):964–971.
- Augustin M, Wilsmann-Theis D, Körber A, et al. Diagnosis and treatment of xerosis cutis - a position paper. J Dtsch Dermatol Ges. (2019);17 Suppl 7:3–33.