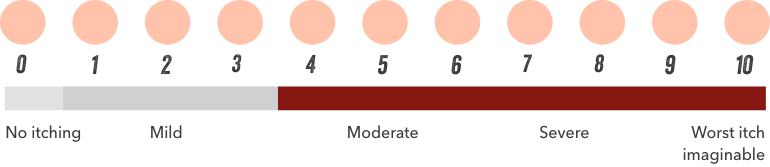
Haemodialysis patients moderately affected by itching had a 1.4–1.6-fold higher adjusted odds of being awake at night, feeling sleepy during the day, or not having enough sleep, compared to patients not bothered by itchy skin.1

Patients with severe (very much and extremely bothered by itching) CKDassociated Pruritus are 2–2.5 times more likely to report suffering from poor sleep quality and 2 times as likely to report feeling washed out or drained than patients not bothered by itching.2